


The top choice to explore the world
Hotels
Flights
New! Whoosh
Trains
Bus & Travel
Airport Transfer
Car Rental
Things to Do
More
One-way / Round-trip
Multi-city
1 Adult, 0 Child, 0 Infant (on lap)
Economy
Looking for
Discover Flight Ideas
Price Alert
10% New User Coupons
Valid for First Transaction on Traveloka App
Save up to 10% for Your First Hotel Booking
Valid for New Users in App Only
JALANYUK
Copy
Save up to 10% for Your First Attractions Booking
Valid for New Users in App Only
JALANYUK
Copy
Save up to 12% for Your First Airport Transfer Booking
Valid for New Users in App Only
JALANYUK
Copy
Save up to 10% for Your First Car Rental Booking
Valid for New Users in App Only
JALANYUK
Copy
Save Rp 25.000 For Your First Bus Booking
Valid for New Users in App Only
JALANYUK
Copy
Save Rp 10.000 For Your First Shuttle Booking
Valid for New Users in App Only
JALANYUK
Copy
Enhance your trip the way you like it
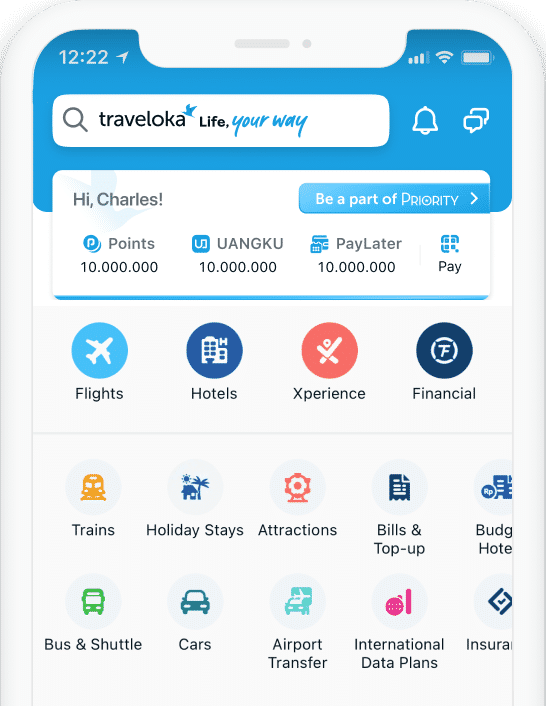
Why book with Traveloka?
50M+ Downloads,
1M+ Reviews
4.6
4.7
Download Traveloka App
App-only deals
Unlock special prices and exclusive app discounts.
Easy refund & reschedule
Adjust your plans with ease, even on the move.
Instant notifications & alerts
Get notified about flight changes and important trip updates.
What interests you?
Popular Flight
Popular Hotel
Popular Activities
Other Popular Products
Tiket Pesawat
Tiket Pesawat ke Bali
Tiket Pesawat ke Singapore
Tiket Pesawat ke Lombok
Tiket Pesawat ke Jakarta
Tiket Pesawat ke Surabaya
Tiket Pesawat ke Kuala Lumpur
Tiket Pesawat ke Malang
Tiket Pesawat ke Medan
Tiket Pesawat ke Jogja
Tiket Pesawat ke Bangkok
Tiket Pesawat ke Hong Kong
Tiket Pesawat ke Semarang
Tiket Pesawat ke Belitung/Tanjung Pandan
Tiket Pesawat ke Malaysia
Tiket Pesawat ke Vietnam
Tiket Pesawat Jakarta-Bali
Tiket Pesawat Jakarta-Padang
Tiket Pesawat Jakarta-Surabaya
Tiket Pesawat Jakarta-Makassar
Tiket Pesawat Jakarta-Lombok
Tiket Pesawat Bali-Jakarta
Tiket Pesawat Balikpapan-Surabaya
Tiket Pesawat Jakarta-Pekanbaru
Tiket Pesawat Jakarta-Pontianak
Tiket Pesawat Jogja-Karimunjawa
Tiket Pesawat Semarang-Karimunjawa
Tiket Pesawat Surabaya-Balikpapan
Tiket Pesawat Surabaya-Bali
Tiket Pesawat Jakarta-Jayapura
Tiket Pesawat Jakarta-Batam
Tiket Pesawat Jakarta-Bandar Lampung
Tiket Pesawat Jakarta-Singapore
Tiket Pesawat Jakarta-Kuala Lumpur
Tiket Pesawat Jakarta-Bangkok
Tiket Pesawat Medan-Kuala Lumpur
Flight Radar
Lion Air
Pelita Air
Susi Air
Citilink
Batik Air
Air Asia
Emirates
Vietravel
KLM
Super Air Jet
Garuda Indonesia
Singapore Airlines
Malaysia Airlines
Japan Airlines
Etihad Airways
Bandara Soekarno-Hatta (CGK)
Bandara Silangit (DTB)
Bandara Yogyakarta International Airport (YIA)
Bandara Changi International Airport (SIN)



Products
Copyright © 2026 Traveloka. All rights reserved

























